Platelet-Rich Plasma (PRP)

Platelet-Rich Plasma is the 3rd topic in my series
about regenerative medicine treating painful musculoskeletal conditions.
This regenerative injection procedure was originally used in 1987 following
open-heart surgery. Ever since then, PRP has gained recognition as a popular
procedure in a variety of medical fields, “including orthopedics, dentistry,
ENT, neurosurgery, ophthalmology, urology, wound healing, as well as cosmetic,
cardiothoracic and maxillofacial surgery.”1 PRP's acceptance and popularity with the
public is partly a result of professional athletes, such as the golfer, Tiger
Woods, and several major league pitchers using the procedure.1
In the practice of orthopedics, “orthobiologics” is understood to be
substances that can facilitate the healing of cartilage, bone, muscle, tendon,
and ligament.2 PRP
is definitely an autologous orthobiologic solution. “Autologous” simply refers to the fact
the solution utilized in the procedure is obtained from the patient.3
PRP is also marketed because of its multiple therapeutic applications
in the field of aesthetics, including wound healing, hair restoration,4 breast
augmentation,5
facial rejuvenation,6 and management of both male7 and female8 sexual dysfunction. A common observation during these studies is
the lack of standardized methods and documentation to aid clinical
outcomes.
PRP is even gaining acceptance in the veterinary world. In the June
2023 issue of Innovative Veterinary Care,9 the authors explain that
“PRP energizes the repair of soppy tissues and joints – and uses the body's own
programming for self-healing with an amplified scale.”
How Does PRP Work?
PRP involves removing a precise quantity of the patient's
own blood and concentrating the platelets, creating a supraphysiologic
concentration of platelets which are then precisely injected to improve
functioning, dependent upon the patient's condition.
When a personal injury happens in a blood vessel, platelets migrate to
the site of harm and form a plug . An ordinary platelet count is 150 000
to 450 000 platelets per microliter
of blood, with an average baseline of 200 000 platelets/uL.10 Studies have demonstrated clinical
benefits using a the least Four times the200
000 platelet/uL
baseline. This is considered the benchmark for “therapeutic PRP”; a count of just one
million/uL is the
standard concentration.1
The advantages of PRP be a consequence of the 3-5-fold concentrate of growth factors and cytokines. Growth factors and mediators promoting regeneration and healing include TGF-1, IGF-1, IGF-B, VEGF, PDGF, bFGF, and EGF. These growth factors play an important role in cell proliferation, chemotaxis, cell differentiation, and angiogenesis.11,12 The healing mechanism of PRP may be the localized inflammatory response that triggers a wound-healing cascade. This leads to the deposition of new collagen in tissues such as tendons and ligaments. The brand new collagen contracts because it matures, providing stability towards the injection site and reduction of pain.11
Figures 1a-d. Platelet Collection for Injection
Figure 1a

60 cc of blood in the patient are transferred to the
concentrating container
Figure 1b

Serum is separated from the RBCs following the first centrifuge
spin
Figure 1c

Platelet plasma following the second centrifuge spin, now in a
different concentrating container
Figure 1d
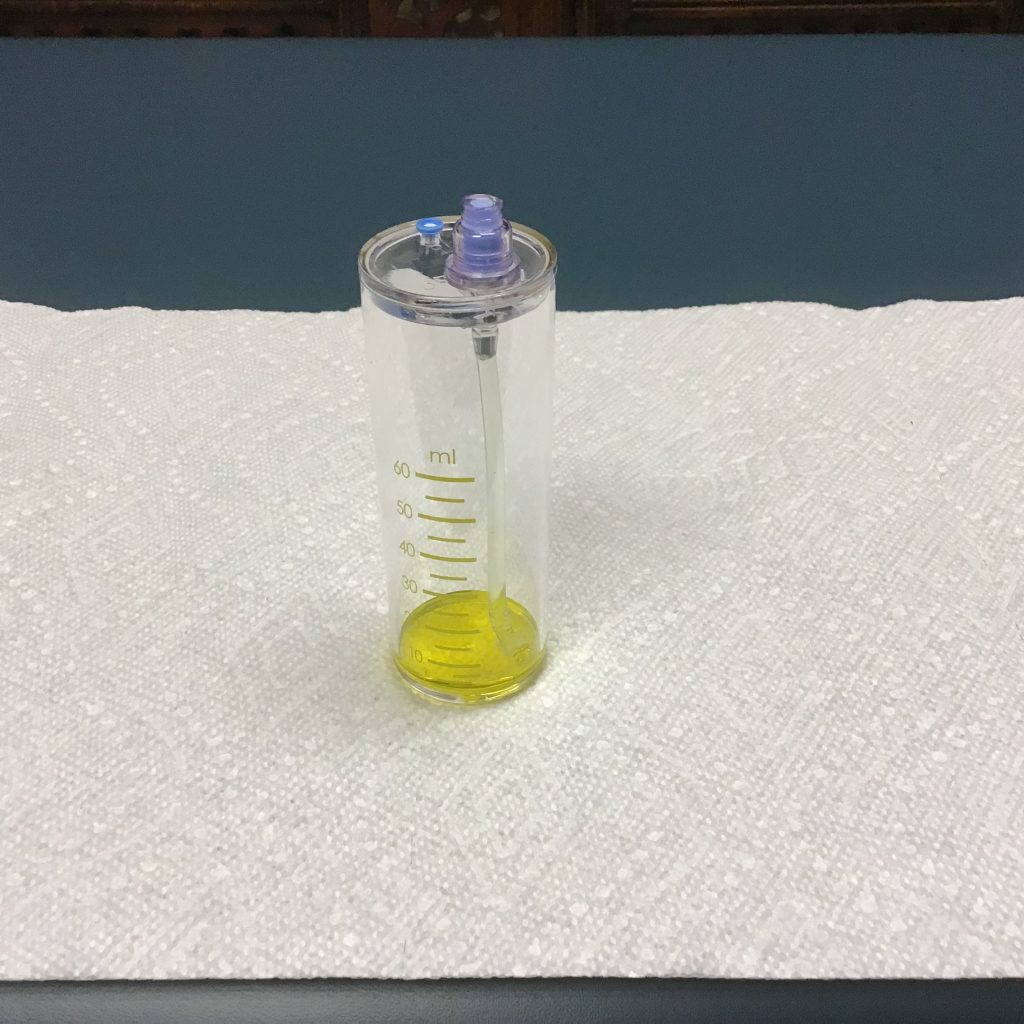
5-10 cc of platelets are separated from the plasma for
injection
There are many different PRP systems, each of which may utilize
another platelet yield concentration. Since there is no standardized PRP
preparation, the practitioner should assess the collection manner in which best
meets his or her practice needs.
Solutions & Applications Aren't Created Equal
PRP Solutions
PRP solutions are influenced by the quantity of blood
taken, the ultimate volume of plasma where the platelets are suspended, the presence
or lack of RBCs and WBCs, the presence or absence of anticoagulant in the
sample, and the addition or absence of thrombin or calcium chloride.13
Lack of great benefit noticed in some studies could be traced to some
variety of factors. Poor-quality PRP can be related to factors such as
inadequate devices or subtherapeutic amounts of platelets.11 As stated by Weibrich et
al, “Advantageous biological effects appear to occur when PRP with a platelet
concentration of approximately 1,000,000/microl is used. At lower
concentrations, the result is suboptimal, while higher concentrations might
possess a paradoxically inhibitory effect.”14
PRP solutions could be further differentiated by leukocyte-rich
PRP vs leukocyte-poor PRP. Because the terms suggest, leukocyte-rich PRP describes a
higher concentration of WBCs , whereas leukocyte-poor PRP refers
to some lower power of WBCs, below baseline. Various scientific studies
support the use of different solutions, dependent upon the region
treated.12
PRP Applications
Dr Gary Clark and also the Hackett-Hemwall-Patterson Foundation
have discussed the importance of Clinical BioTensegrity within the management of
painful musculoskeletal conditions.15 Following a principals of BioTensegrity
with PRP when treating a painful knee, for example, multiple areas would be
injected, such as the intra-articular joint and extra-articular structures,
such as the patellar tendon, quadriceps tendon, medial collateral ligament,
lateral collateral ligament, and pes anserine tendons.
There is consensus within the literature for a standard protocol for PRP preparation and application.16 Multiple investigators have concluded that further research is required to properly measure the efficacy of PRP treatment to produce optimum benefit based on evidence-based guidelines.17-20 Based on a current Chinese study, “A large, multicenter, randomized trial is needed to further assess the efficacy of PRP strategy to patients with knee OA.”16 And the authors of the 2023 review recommend that future research focus on “the ideal type, dose, frequency of injection and mode of injection.”21
Table 1. Common Musculoskeletal Conditions Treated with PRP
| Achilles tear | Hip pain & arthritis | Rotator cuff tears |
| Achilles tendonitis |
Joint laxity & instability |
Rotator cuff tendonitis |
|
Ankle pain & arthritis |
Knee pain & arthritis |
Sacroiliac joint pain |
| Ankle sprains | Knee ligament injuries | Sciatica |
| Cartilage damage | Knee tendonitis |
Shoulder pain & arthritis |
|
Cervical radiculitis |
Ligament tear |
Spinal disc problems |
|
Elbow pain & arthritis |
Low lower back pain | Sprains & strains |
| Elbow tendonitis | Neck pain | Tendonitis |
| Foot pain & arthritis | Patellar tendonitis | Thoracic pain |
| Golfer's elbow | Pelvic pain | Tennis elbow |
| Hand pain & arthritis | This problem |
Wrist pain & arthritis |
PRP Studies
Varying outcomes are reported in the literature regarding
the potency of PRP for various conditions:
- Knee osteoarthritis:
Inside a 2023 systematic overview of 14 randomized controlled trials including
1423 participants, the investigators figured intra-articular knee PRP
injections “probably tend to be more efficacious within the treatment of knee OA
in terms of pain alleviation and self-report function improvement
at 3, 6, and 12 months follow-up, in contrast to other injections, including
saline placebo, HA, ozone, and corticosteroids.”22 Another systematic review found significant
clinical improvements in knee osteoarthritis treated with PRP.23 - Tendinopathy:
A 2023 meta-analysis, including 18 studies and 1066 participants, examined the
effectiveness of PRP for tendinopathy, using the primary outcome measure
being alternation in pain intensity.24 The authors concluded, “There is nice evidence to
support the utilization of leukocyte-rich PRP under ultrasound guidance in
tendinopathy. Both preparation and intratendinous injection technique of PRP
seem to be of great clinical significance.” - Musculoskeletal
injuries: A 2013 review, including randomized and quasi-randomized
controlled trials, evaluated PRP for soft-tissue injuries.25 The primary
outcomes were functional status, pain, and adverse effects. PRP was compared to
placebo, autologous whole blood, and dry needling. Based on the authors, “[T]here
is currently insufficient evidence to support using [platelet-rich
therapies] for treating musculoskeletal soft tissue injuries.”25 - Sports injuries:
In a 2023 systematic review and meta-analysis of 13 RCTs, the authors concluded
that PRP was no more effective for sports-related injuries than other
treatment options.18
Because there is certainly no standardization for the PRP
solution and application, the clinical connection between PRP treatment vary widely.
Results are affected by a number of different factors:
- clinical use of PRP, ie, what it's
being used to deal with - the quantity of injection areas treated
- the number of actual injections
- ultrasound-guidance using the injections
- the PRP and leukocyte concentration
- the frequency of application
Case History
A 72-year-old female patient given chronic left groin, hip and leg pain. I administered ultrasound-guided injections of PRP and ozone to the left hip . It is not easy to understand the degree of moderate-to-severe osteoarthritis in this ultrasound image. The joint capsule is enlarged in this picture following ultrasound-guided injections of PRP and ozone.
Figure 2. Ultrasound Picture of Left Hip after Injections

Figure 3 is definitely an X-ray of the patient's pelvis and left hip joint more clearly illustrates the moderate-to-severe osteoarthritis from the left hip joint; it also demonstrates the asymmetry from the pelvis. I treated the patient's left hip with 1 ultrasound-guided prolotherapy treatment and 3 separate ultrasound-guided PRP treatments, each 30 days apart. The patient responded perfectly to her treatments, reporting significant pain reductions in her left hip, groin, and left leg. She seemed to be referred to a chiropractor for treatment of the pelvic misalignment.
Figure 3. A-P X-ray of Pelvis & Lumbar Spine

PRP Combinations
Combinations of PRP with gels, scaffolds, and/or stem
cells represent exciting applications worthy of exploration. Different studies,
for instance, show the advantages of combining PRP with bone marrow aspirate
concentrate 26
or amniotic allograft.27
Dr Frank Shallenberger recommends combining PRP and ozone for
all PRP applications.28
I administer ozone after all my PRP injections. Even though the manner of combining
PRP with regenerative solutions such as alpha-2-macroglobulin or exosomes can
be located on various practitioners' websites, evidence falls short of the
literature as to its effectiveness.
Patient Selection, Evaluation, & Safety
As with any regenerative joint procedure, PRP isn't a
remedy for all painful musculoskeletal conditions. Practitioners must be
realistic in their selection of each case. Before treatment, each patient should
be evaluated with an individual basis having a through history, physical exam with
relevant orthopedic tests, and diagnostic testing, which commonly includes X-rays,
MRIs, ultrasound evaluation, and full laboratory work-up.
PRP & Ultrasound
Compared to other regenerative solutions, such as
prolotherapy and prolozone, PRP is more epensive and the amount of solution is
limited. Consequently, using ultrasound to steer injections is particularly valuable
for achieving precise needle placement, specifically for deeper injections.
Learning PRP
The same principals practiced in prolotherapy and
prolozone also affect PRP. For instance, the start regenerative medicine
practitioner should stick to the same steps to learn human body as recommended
for other regenerative joint injections. Some of the more commonly recognized
organizations that teach injection procedures include the American Osteopathic
Association of Prolotherapy Regenerative Medicine, the American Association of
Osteopathic Prolotherapy, and the Hackett-Hemwall-Patterson Foundation. The
Neil Riordan Regenerative Medicine Center at Southwest College of Naturopathic
Medicine also offers prolotherapy training to doctors, which includes
both lecture and “hands-on” injection experience.
Summary
PRP is an autologous, orthobiologic product that comes from the patient's own blood. It is a safe, natural, non-drug, non-surgical treatment that harnesses the body's healing power to stimulate collagen tissue regeneration and strengthen weakened ligaments and tendons. You will find inherent healing growth factors in PRP that stimulate tissue regeneration. There's a wide variety of treatment applying PRP in orthopedics, aesthetics, and men and women sexual function. There's a definite requirement for standardization regarding its use, to achieve optimum therapeutic benefit. The clinical results of PRP depends upon both the PRP solution and application. Although the reported efficacy of the treatment varies in the literature, this regenerative medicine method has repeatedly demonstrated successful outcomes for various conditions. The patient should be properly selected and evaluated to ensure optimum outcome. The practitioner should have an in-depth knowledge of anatomy and also have taken time to build up palpation skills. It is primarily the author's opinion that PRP should be considered as a logical first step in the management of musculoskeletal conditions before considering surgery, including joint replacement.