Case Study: Herbal Treatment of Depression

Vis Medicatrix Naturae
Depression is one of the most typical mental health disorders seen in clinical practice. In 2023, approximately 16.A million adults in america had experienced at least 1 major depressive episode in the past year.1 The lifetime prevalence of depression for adults in the US is estimated to be 16%.2 A variety of socioeconomic factors have been associated with an increased risk for depression, including middle-age, a femeale, Native American ethnicity, lower income status, unemployment, being single or divorced, and having a disability.1
The DSM-IV defines major depressive disorder as more than 2 episodes consisting of depressed mood along with a loss of interest in usually pleasurable activities that occurs most days throughout a minimum of 2 weeks. Other possible symptoms include fatigue, alterations in sleeping or eating patterns, feelings of low self-esteem and self-worth, diminished concentration, and recurrent thoughts of self-harm and death.3
Conventional treatment of MDD typically consists of psychotherapy and pharmaceuticals.4 The effectiveness of various classes of antidepressants is similar, with response rates in numerous studies varying from 50% to 75%,5 and appears to become correlated with the initial severity of depressive symptoms: Clinically significant improvements are more likely in severe and chronic depression, and benefits in many cases are negligible in mild-to-moderate depression.6 Despite their possible benefits, many patients are cautious about antidepressants, citing concerns about adverse side effects, including fatigue, sleep disturbances, weight gain, gastrointestinal distress, and loss of libido.
Fortunately, naturopathic medicine offers many powerful modalities for patients with mood disorders including botanical therapies, nutraceuticals, homeopathy, flower essences, nutritional interventions, and stress management techniques. For patients with mild-to-moderate depression or people who prefer to avoid pharmaceutical approaches, well-chosen natural treatments might be an appropriate and efficient option.
Case Study
Sue is really a 45-year-old female who given to my clinic in June 2023 for difficulties with fatigue and foggy thinking. At our first office visit, she rated her degree of energy as variable, ranging from Three to six out of 10. She stated that, after a few hours of exercise, she was often overcome by exhaustion. She also described frequent insomnia. Sue commonly delayed bedtime until she was completely exhausted, falling asleep around midnight and waking between 6:00 and eight:00 AM on most days.
Sue reported persistent and significant anxiety, which had plague her since childhood. During episodes of anxiety, she experienced the signs of muscle tension in her own shoulders, neck, and jaw. Although she'd experienced multiple episodes of depression in her lifetime, at the time she came to see me, she said she wasn't experiencing depressive symptoms. She expressed worry about the results that chronic stress might have on her behalf all around health.
Sue's diet was basically a typical American diet. She explained that her diet would suffer during bouts of depression. Her water intake was approximately 75 to 100 ounces water daily and she did not are drinking alcoholic beverages or caffeinated beverages. Sue was not exercising regularly but she was physically active during the day, and discussed a wish to restart a house yoga practice. Significant findings on review of systems included intermittent tension headaches and migraines.
Her past health background was significant for chronic post-traumatic stress disorder following repeated sexual abuse. She had also experienced multiple traumatic brain injuries . Sue reported a 16-month period starting in 2010 when she was frequently disassociating. She was often not able to eat or leave her house during this period coupled with trouble performing activities of daily living. She also reported intermittent episodes of vomiting and intense physical pain, which she related to somatic expressions of psychological pain. Sue had been unemployed for several years and was currently single and living alone.
Sue had been in counseling intermittently for well over a decade, and reported that she had tried multiple antidepressants with no success. Actually, the majority of the medications worsened her depression and caused weight gain. The only real medication she'd discovered to be helpful would be a drug containing amphetamine plus dextroamphetamine , that's prescribed for issues with cognition and concentration following a TBIs. At the time she found see me, Sue was using Piper methysticum at a dose of 500-1000 mg PRN, up to BID, for anxiety. She seemed to be supplementing with methylcobalamin and cholecalciferol.
I ordered an extensive variety of diagnostic tests and prescribed 350 mg of a magnesium at bedtime and advised her to continue taking her current dose of Piper methysticum as required for anxiety.
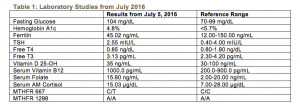
Sue's laboratory testing revealed a heterozygous 677C/T MTHFR polymorphism, and a low-normal 25-OH vitamin D level despite daily supplementation. Her fasting glucose was mildly elevated at 104 mg/dL, however HbA1c was optimal at 4.8%. Her CBC, CMP, ferritin, lipids, cortisol, and thyroid studies counseled me otherwise within normal limits. Complete results of these laboratory studies are presented in Table 1. I prescribed a short-course of high-dose vitamin D3 along with a multivitamin containing 800 mcg of L–5–Methyltetrahydrofolate, 1000 mcg of vitamin B12, activated types of other Vitamin b, and trace minerals. The patient reported that magnesium was helping to improve her sleep quality and quantity and she was sleeping a minimum of 8 hours every night.
At our 1-month follow-up, Sue said that she had been experiencing depressed moods. She described profound sadness, hopelessness, along with a sense that her “future was bleak,” but said she was not having suicidal ideations. She was struggling with a lack of motivation and described needing 2 hours to get away from bed within the mornings. She stated that she was “numbing” her moods with television and overeating. She seemed to be less careful to include protein and vegetables at meals.
Goals of Treatment
The goal of treatment in MDD is to assist the patient go back to full functioning and a high quality of life. Remission is understood to be a minimum of 30 days absent sad mood and anhedonia, without any a lot more than 3 remaining the signs of a major depressive episode.7 The prognosis for MDD is highly variable. Approximately 20% of individuals will experience a recurrence within the first Six months following recovery from the major depressive episode. Furthermore, between 50% to 85% of people may have at least 1 recurrence, usually within 2 -3 years of the first depressive episode.1
For the numerous patients who experience chronic or recurrent depression, pragmatic goals ought to be centered on decreasing the severity and frequency of episodes. Improvements can be measured subjectively throughout the patient interview and by utilizing clinical tools such as the Patient Health Questionnaire-9 or Hamilton Depression Rating Scale .
Herbal Prescriptions
A growing body of studies show that herbal supplements can be a safe and effective in the management of MDD along with other mood disorders. The greatest results may be had when herbal treatments are carefully individualized and adapted to changing needs as the clinical picture changes.
I prescribed a natural formula to support the adrenal glands and nervous system containing Avena sativa, Melissa officinalis, Scutellaria lateriflora, Panax quinquefolius, and Rhodiola rosea. This formula was chosen in part to deal with her past record of PTSD and TBI. 1 week later, the patient reported that her energy had improved within a few days of starting the tincture and she was beginning to wake feeling refreshed.
When another episode of MDD occurred, I added a second botanical formula, which contained Hypericum perforatum, Actaea racemosa, Verbena hastate, and a few drops of a Love-Lies-Bleeding flower essence. Flower essences could be a gentle yet powerful accessory for a natural tincture. They're highly individualized to a particular kinds of mood concerns and could assistance to address the emotional and spiritual imbalances and traumas underlying an individual's experience. I've found that lots of patients appreciate being involved with choosing flower essences to increase their treatment.
Two weeks later, the individual reported general improvements in depressed and anxious moods, particularly when she was consistent with the tinctures. She noted that her headaches were also considerably less frequent when she was compliant with treatment. She reported increased feelings of calm and serenity and an capability to pay attention to her inner needs. She stated that her energy continued to be variable and seemed to directly correlate with her moods.
At subsequent visits the patient reported occasional worsening of mood, sleep, and energy that were triggered by significant life stressors and impending transitions in her life. She was still being bothered by her general insufficient energy; therefore, I prescribed another dietary supplement containing Lepidium meyenii, Withania somnifera, Glycyrrhiza glabra, Oplopanax horridus, and Olive flower essence. We continued to discuss stress management techniques and the ways to reframe her experience of depression. I additionally encouraged her to begin treatment with a psychotherapist trained in Eye Movement Desensitization and Reprocessing , which she reported to be very helpful.
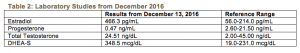
At our 6-month follow-up, Sue's mood was greatly improved, but she was continuing to experience intermittent fatigue. Although she described regular cycles and normal menses, Sue requested hormone testing, which revealed elevated serum DHEA-S and estradiol levels, and a low-normal progesterone level on day 30 of her menstrual period. Complete results of these tests can be found in Table 2. I made a decision to get rid of Glycyrrhiza, which could contribute to the elevated DHEA-S,8 as well as Lepidium and Actaea, which may have estrogenic actions,9,10 from her protocol, and prescribed 2 new formulas: the very first contained Hypericum perforatum, Verbena hastate, and Scutellaria lateriflora; the 2nd contained Rhodiola rosea, Ocimum sanctum, Withania somnifera, and Vitex agnus-castus. The patient was then lost to follow-up as she had moved out of state, but she was strongly encouraged to follow through with repeat hormone testing and also to re-establish care having a psychotherapist.
A Closer Look at Nervine Herbs
Nervine herbs should be thought about as a foundational aspect of mood disorder treatment. They nourish and calm the nervous system and therefore are particularly important when stress, irritability, trauma, or anxiety exists. These herbs can be quite helpful in restoring emotional balance.
Hypericum perforatum is an organic herb traditionally indicated for neuralgic pain and viral infections, however it has additionally become One of the most widely used natural treatments for depression. In herbal folklore, Hypericum perforatum has been said to “let the sun's rays shine in” because of its doctrine of signatures wherein the leaves from the plant have small perforations. Clinical studies have shown Hypericum to be effective for the treatment of mild-to-moderate MDD. In fact, Hypericum extracts might have better response and remission rates than antidepressants for example paroxetine within the treatment of moderate MDD.11 Hypericum has also been proven to possess a favorable side-effect profile and tolerability in comparison with antidepressant medications.12 Early research has suggested that Hypericum inhibits monoamine oxidase A ;13 other studies, however, have refuted this finding.14 The antidepressant action of Hypericum are closely related to the capability to increase serotonin production by inhibiting tryptophan 2,3-dioxygenase activity.15 The best clinical concern when prescribing Hypericum is potential herb-drug interactions, since Hypericum has been discovered to be a potent inducer of cytochrome P450 enzymes and of P-glycoprotein.11
Avena sativa is a trophorestorative chosen to address the history of prolonged stress and TBI. Avena is indicated for nervous exhaustion, melancholy, and diminished mental concentration.16 Avena has been found to affect neural activity in the region of the brain involved in cognition in healthy individuals, and may have a positive impact on cognition.17
There are unfortunately few research on Verbena hastate , however it includes a long-standing use within traditional herbal medicine as a nervine and antispasmodic. Verbena is indicated for exhaustion and nervous depression and it is specific for people who suppress their emotions and frustrations.16 Scutellaria lateriflora is indicated for stress and anxiety, especially if you find a powerful feeling of overwhelm and oversensitivity.18,19 Scutellaria is also used to treat restless sleep and dull frontal headaches.16 Melissa officinalis is often referred to as the “gladdening herb.” It is useful for nervous depression, particularly when there's debility or weakness following chronic stress.20
A Closer Look at Adaptogenic Herbs
For those who experience MDD, it is common for a lifetime stressors to become a trigger for depressive episodes.Insufficient motivation and low energy will also be a substantial concern for most people struggling with MDD.Because adaptogens have potent effects around the neuroendocrine system, and lots of will also be immune modulators, these herbs are a good option for many patients with MDD.
Withania somnifera is definitely an Ayurvedic herb traditionally considered anti-inflammatory, anti-rheumatic, and adaptogenic. Withania is amphoteric in its action, as it can both stimulate and relax the nervous system; it's indicated for insomnia, fatigue, and debility brought on by chronic stress.21 Over 35 chemical constituents of Withania have been studied, including alkaloids, steroidal lactones, saponins, and withanolides.22 Clinical trials claim that it decreases serum cortisol levels and improves self-reported quality of life in people experiencing chronic anxiety and stress.23
Lepidium meyenii is really a medicinal food native to the Peruvian Andes. Although primarily studied for its effects on menopausal climacteric symptoms and infertility, animal studies claim that Lepidum also has antidepressant and anxiolytic effects. Lepidium may act to regulate the hypothalamic -pituitary -adrenal axis, increasing dopamine and norepinephrine levels in the brain while also decreasing serum cortisol. It's also been shown to reduce oxidative stress within the brain. Increased levels of reactive oxygen species have been found in the plasma and brains of individuals with MDD, thus suggesting that oxidative stress may be a contributor to depression.24
Glycyrrhiza glabra has extensive and varied uses in lots of systems of drugs. Glycyrrhiza is anti-inflammatory, phytoestrogenic, and memory-enhancing, also it might help to relieve fatigue.25,26 Studies have shown that Glycyrrhiza has mineralcorticoid properties and increases circulating amounts of unconjugated deoxycorticosterone, dehydroepiandrosterone , and testosterone. This seems to be due to its glycyrrhetinic acid, a constituent that inhibits 11β-hydroxysteroid dehydrogenase type 2, an enzyme that is active in the inactivation of glucocorticoids.8
Oplopanax horridus is an herb native to the Pacific Northwest. Oplopanax is a member of the Araliaceae family, of which the greater familiar Panax quinquefolius is additionally a member. Although dammarane saponins are not present in any Oplopanax, it will contain various other triterpene glycosides.27 Oplopanax is traditionally considered a protective plant ally and it is indicated for shy, timid folks who suffer from difficulty adjusting to stressful situations.16
Discussion
The United States Preventative Services Task Force recommends that adults and adolescents be screened annually for depression during primary care visits. A common screening tool is the 2-question PHQ-2. If positive, this should then trigger further evaluation while using PHQ-9, HAM-D, or any other depression symptom inventory. Depression screening should be accompanied by appropriate treatments, referrals, and follow-up.28
Treatment of despression symptoms frequently requires an individualized, holistic, and integrative approach. Naturopathic prescription medication is especially well suited for the treatment of depression because of the many modalities open to practitioners. A comprehensive naturopathic treatment for depression can include using nervine and adaptogenic herbs, flower essences, nutraceutical supplements, lifestyle and diet modifications, and an appropriate referral for psychotherapy.
[References]
- Bose J, Hedden SL, Lipari RN, Park-Lee E. Key substance use and mental health indicators in the usa: Results from the 2023 National Survey on Drug Use and Health. Substance Abuse and Mental Health Services Administration. https://www.samhsa.gov/data/sites/default/files/NSDUH-FFR1-2023/NSDUH-FFR1-2023/NSDUH-FFR1-2023.pdf. Published September, 2023. Accessed January, 2023.
- Kessler RC, Berglund P, Demler O, et al. The epidemiology of major despression symptoms: is a result of the National Comorbidity Survey Replication . JAMA. 2003;289:3095 -3105.
- Center for Substance Abuse Treatment. Managing Depressive Symptoms in Drug abuse Clients During Early Recovery. Drug abuse and Mental Health Services Administration. https://www.ncbi.nlm.nih.gov/books/NBK64057/. Published 2008. Accessed January 19, 2023.
- American Psychiatric Association. Practice Guideline for the Management of Patients with Major Depressive Disorder, 3rd ed. National Guideline Clearinghouse. https://www.guideline.gov/summaries/summary/24158/Practice-guideline-for-the-treatment-of-patients-with-major-depressive-disorder-third-edition. Published October 2010. Accessed January, 2023.
- Linde K, Kriston L, Rucker G, et al. Efficacy and acceptability of pharmacological treatments for depressive disorders in primary care: Systematic review and network meta-analysis. Ann Fam Med. 2023;13:69 -79.
- Fournier JC, DeRubeis RJ, Hollon SD, et al. Antidepressant drug effects and depression severity: A patient-level meta-analysis. JAMA. 2010;303:47 -53.
- Rush AJ, Kraemer HC, Sackeim HA, et al. Report by the ACNP Task Force on response and remission in major depressive disorder. Neuropsychopharmacol. 2006;31:1841 -1853.
- Al-Dujaili E, Kenyon C, Nicol M, Mason J. Liquorice and glycyrrhetinic acid increase DHEA and deoxycorticosterone levels in vivo and in vitro by inhibiting adrenal SULT2A1 activity. Mol Cell Endocrinol. 2011;336:102 -109.
- Meissner HO, Mscisz A, Reich-Bilinska H. Hormone-balancing effect of pre-gelatinized organic maca. Int J Biomed Sci. 2006;2:375 -394.
- Powers CN, and Setzer, W. A molecular docking study of phytochemical estrogen mimics from dietary herbal medicines. In Silico Pharmacol. 2023;3.
- Seifritz E, Hatzinger M, Holsboer-Trachsler E. Efficacy of Hypericum extract WS 5570 in contrast to paroxetine in patients with a moderate major depressive episode – a subgroup analysis. Int J Psychiatr Clin Prac. 2023;20:126 -132.
- Apaydin EA, Maher AR, Shanman R, et al. An organized overview of St. John’s wort for major despression symptoms. Syst Rev. 2023 2;5:148.
- Suzuki O, Katsumata Y, Oya M, et al. Inhibition of monamine oxidase by hypericin. Planta Med. 1984; 50:272 -274.
- Julia Sacher, MD, PhD, Sylvain Houle, MD, PhD, Jun Parkes, MSc, et al. Monoamine oxidase A inhibitor occupancy during management of major depressive episodes with moclobemide or St. John's wort: an [11C]-harmine PET study. J Psychiatry Neurosci. 2011; 36:375 -382.
- Bano S, Ara I, Saboohi K, et al. St. John’s Wort increases brain serotonin synthesis by inhibiting hepatic tryptophan 2, 3 dioxygenase activity and its gene expression in stressed rats. Pak J Pharm Sci. 2023;27:1427 -1435.
- Tilgner S. Herbal medicine: from the heart from the earth. Creswell, OR: Wise Acres; 1999.
- Dimpfel W, Storni C, Verbruggen M. Ingested oat herb extract changes EEG spectral frequencies in healthy subjects. J Alternt Complement Med. 2011;17:427 -434.
- Brock C1, Whitehouse J, Tewfik I, Towell T. American Skullcap : a randomized, double-blind placebo-controlled crossover study of their effects on mood in healthy volunteers. Phytother Res. 2023;28:692 -698.
- Wood M. The earthwise herbal: an entire help guide to New World medicinal plants. Berkeley, CA: North Atlantic Books; 2009: 323 -325.
- Wood M. The earthwise herbal: an entire help guide to ” old world ” medicinal plants. Berkeley, CA: North Atlantic Books; 2009: 342 -344.
- Thorne Research, Inc. Monograph: Withania somnifera. Altern Med Rev. 2004 Jun;9:211 -214.
- Mishra LC, Singh BB, Dagenais S. Scientific Basis for the therapeutic use of Withania somnifera : A Review. Altern Med Rev. 2000;5:334 -346.
- Chandrasekhar K, Kapoor J, Anishetty S. A prospective, randomized double-blind, placebo-controlled study of safety and efficacy of a high-concentration full-spectrum extract of ashwagandha root in lessening stress and anxiety in grown-ups. Indian J Psychol Med. 2012;34:255 -262.
- Ai Z, Cheng AF, Yu YT, et al. Antidepressant-like behavioral, anatomical, and biochemical effects of petroleum ether extract from maca in mice exposed to chronic unpredictable mild stress. J Med Food. 2023;17:535 -542.
- Shang H, Cao S, Wang J, et al. Glabridin from Chinese herb licorice inhibits fatigue in mice. Afr J Tradit Complement Altern Med. 2010;7:17 -23.
- Simmler C, Pauli GF, Chen SN. Phytochemistry and Biological Properties of Glabridin. 2013; 90:160 -184.
- Calway T, Du GJ, Wang CZ, et al. Chemical and pharmacological studies of Oplopanax horridus, a United states botanical. J Nat Med. 2012;66:249 -256.
- Siu AL; US Preventive Services Task Force , Bibbins-Domingo K, Grossman DC, Baumann LC, et al. Screening for depression in adults: US preventive services task force recommendation statement. JAMA. 2023;315:380 -387.